Author: Olga Goralewicz, ACT Specialist
Telling the difference between ACT and CBT may be confusing. Both are rooted in behavior therapy. While traditional CBT focuses on eliminating unpleasant feelings and emotions, ACT concentrates on their acceptance.
The second approach works to improve the quality of life while recognizing that not all sensations are pleasant or should be eliminated.
Nonetheless, psychotherapy, as understood by both ACT and CBT, may have similar outcomes.
Key differences between ACT and CBT
- CBT focuses on identifying and changing unhelpful thought patterns and behaviors, while ACT encourages accepting uncomfortable thoughts and feelings as a natural part of life.
- CBT is typically short-term and goal-oriented, targeting specific issues. ACT is an ongoing process meant to be integrated into daily life.
- In CBT, the therapist takes a more directive role in guiding cognitive restructuring. With ACT, the work is more collaborative between client and therapist.
- CBT aims to reduce symptoms, while ACT sees symptom relief as a side effect of living according to one’s values.
- CBT emphasizes changing thoughts to change emotions and behavior. ACT focuses on developing psychological flexibility through mindfulness and committed action aligned with values.
- CBT is older and has more robust research support, while ACT is a newer “third-wave” therapy that incorporates mindfulness techniques.
- CBT works by modifying dysfunctional thoughts related to insomnia, while ACT focuses on accepting present moments and living according to values without judgment.
| Acceptance and Commitment Therapy (ACT) | Cognitive Behavioral Therapy (CBT) |
|---|---|
|
|
Keep reading to learn more details on the differences between CBT and ACT and how these approaches to behavior therapy work in practice.
Cognitive Behavioral Therapy (CBT)
Traditional Cognitive Behavioral Therapy (CBT) comprises a group of psychotherapy techniques and approaches. These target thoughts, sensations, and actions that are considered negative or destructive. Treatment is geared towards change through classical conditioning principles.
The therapist plays an active role to help you recognize thought patterns that have a negative influence on your behavior and emotions. Those are then challenged to come up with objective ones that help eliminate symptoms of disorders like anxiety and depression.
This form of cognitive therapy is often a short-term treatment used to target a specific problem by pushing forward positive thoughts related to the present moment. CBT is highly goal-oriented and focused on change. So, it is necessary to change both thinking (cognition) and what you do (behavior) at the same time. Key strategies include:
- practising new skills,
- setting goals,
- problem-solving,
- self-monitoring, and
- gradual progress.
For example “I missed my deadline, I am completely worthless” can become “I didn’t do my best to meet the deadline, but there is a reason the task was given to me and I will do better next time.”
Acceptance and Commitment Therapy (ACT)
Acceptance and Commitment Therapy works to improve the quality of life while accepting that not all thoughts and beliefs are pleasant or should be eliminated. It comprises 6 core principles and mindfulness skills that patients learn to integrate into everyday life.
It is also considered and based on behavioral therapy. It was created by Steve Hayes in 1986. It belongs to the so-called “third wave” of behavioral therapies.
Those all began in the late 80s, along with
- Dialectical Behaviour Therapy (DBT),
- Mindfulness-Based Cognitive Therapy (MBCT), and
- Mindfulness-Based Stress Reduction (MBSR).
All of those are based on acceptance and mindfulness instead of altering thoughts by force.
Relational Frame Theory (RFT), which was developed a little earlier, is ACT’s own basic research program into human language and cognition. It argues that we learn communication by interaction with the environment and others, and not just on the basis of stimuli links.
Acceptance and Commitment Therapy is relatively new, but the past decade has already provided a lot of promising empirical and clinical data and research supporting claims of its effectiveness in treating disorders like anxiety and depression.
In ACT, symptom reduction is not a goal but rather a desired side-effect. The assumption is that focusing on negative thoughts and actions is what leads to a disorder in the first place. It, therefore, opposes the belief that there is a “healthy normality” but rather builds on the understanding that the human psyche is not inherently void of negative experiences.
ACT treatment is commonly used with individual patients as well as couples and groups. It is effective as both short-term and long-term therapy. There is no exact protocol.
Therapists often come up with mindfulness techniques based on the issue that is being targeted. You as a client have a much larger influence on what those strategies include. This model of cognitive therapy is highly personalized. There are six core principles used to train psychological flexibility.
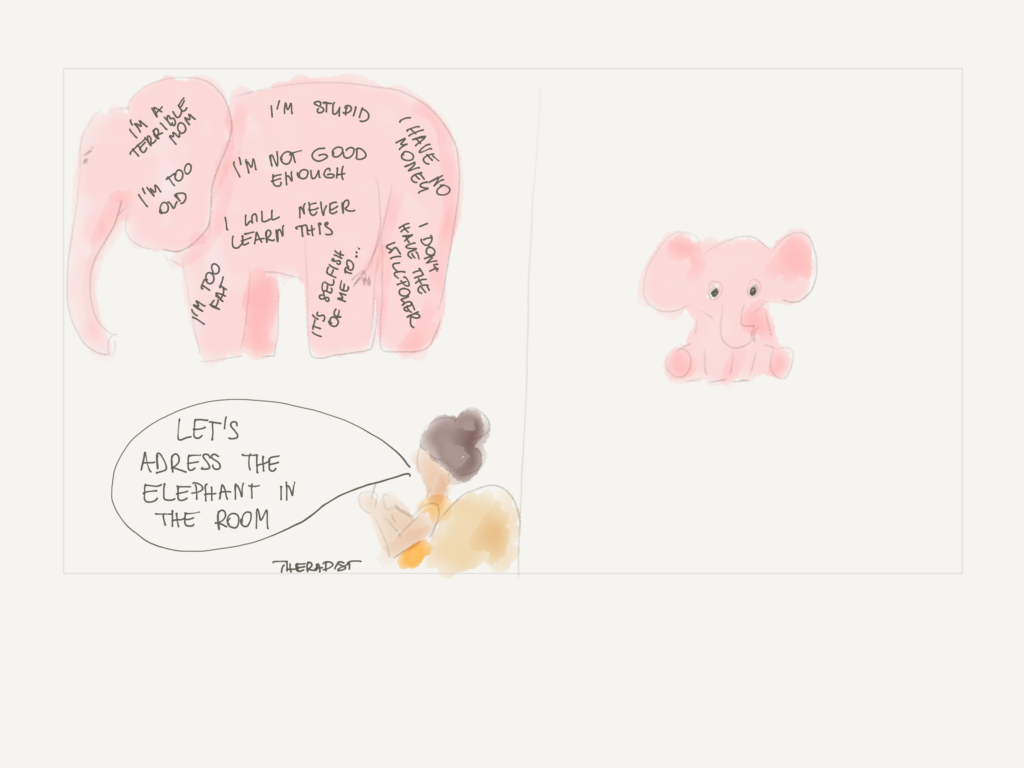
Cognitive defusion
The aim of this ACT strategy is to learn to look at thoughts “from the outside”. Instead of personifying them as things that are threatening or stressful, you are instructed to study them in different ways until they lose the emotional impact.
One way to do this is to picture a phrase such as “I’m boring” as not an immaterial thought, but as if it was no more than words on a screen. You can then alter what those words look like and the way you feel about them may change. This may reduce anxiety someone feels when the thought is unprocessed and acts as a belief.
Acceptance
As the name suggests, this principle is at the center of ACT. The goal is to accept negative feelings that you have no control over. Imagining situations that bring on anxiety and accepting them is one of the most important techniques.
This form of psychological awareness allows for breaking a vicious circle of worrying about things that make us anxious. Accepting that you can’t just get rid of unpleasant feelings makes them easier to digest and process.
It is at this stage that many report changes. The side-effect of feeling less anxiety may become apparent.
Contact with the present moment
Being mindful is also one of the more important goals of ACT treatment. You are encouraged to use all of your five senses to bring yourself into the present moment. That way it is easier to ignore thoughts and impressions that distract us easily. You don’t have to force yourself to not engage with them; this is very difficult. Instead, you let them come and go.
In order to do this, you can try to do things in slow motion. For example, while you are having a conversation and feel yourself dissociating, try to focus on what you hear. Different thoughts may come into your mind, but the goal is to acknowledge them and get back to the present.
The Observing Self
Now we are getting to the more abstract of ACT techniques. The Observing Self is a strategy to help you distance yourself from your thoughts, memories, urges, sensations, images, roles, or physical body. They are not you.
Try to picture your feelings or thoughts. This separates you from them; you are the observer. From this perspective, none of the phenomena is threatening or dangerous. They come and go and are not necessarily based on what is happening.
Values
In the spirit of ACT, one of the first things you can do is assess what your values are. And this means your values, not the values of others. By focusing on what kind of person you want to be, you may become more willing to adjust your behavior and experience feelings of anxiety.
An example would be, let’s say, you want to be more caring towards others. This requires you to reach out to other people, which is a common source of stress. If the psychological reward is that you are more content with yourself, you are more likely to welcome anxiety that appears in the process.
Committed action
Once you set your values, you can commit to achieving related goals. Knowing what is important to you makes it easier to decide how you want to achieve it. The feeling of anxiety will arise, but it shouldn’t be new at this point that the sensation will come and go. In fact, this step is based on all of the principles above coming together.
You will be encouraged to expose yourself to things that caused anxiety previously but in a controlled way. You won’t have to go out of your way to place yourself in uncomfortable situations. Only when the psychological reward of being true to a value is more promising than the feeling of anxiety is threatening.
Is ACT therapy effective?
A randomized controlled study from 2002 found that only 4 hours of Acceptance and Commitment Therapy treatment helped re-hospitalization rates of schizophrenic individuals to drop by 50% over a period of 6 months. (research by Bach, Hayes).
What’s more, over 300 randomized controlled trials were performed, showing overwhelmingly positive results. Hayes and his team started from the ground up. The concepts and techniques they developed are clinically effective and consistent with existing models.
How can I help you using ACT?
You may find the clinical outcomes of either of the therapies successful, no matter whether your therapist chooses to go with ACT or CBT. Many actually start out with CBT (it’s older – more therapists are trained in CBT), and, after not achieving their desired goals, move onto ACT. Behavioral science shows that the former is a good stepping stone.
Both approaches to psychotherapy are worthwhile, but the difference with ACT is that you get to know your body and how to use it for mental purposes. Learning acceptance and self-compassion is something that takes this type of therapy to the next level.
Acceptance and Commitment Therapy encourages you to be present in the moment and teaches you how to keep such behavior up in every area of life. Drastic changes in behavior are not necessarily the goal. It is more about how you feel about the behavior you are already familiar with.
As mentioned above, ACT addresses “experiential avoidance”. If you accept that stressful situations cause you anxiety, rather than avoiding such situations or forcing yourself to calm down, you will build a relationship with this feeling. The premise is that concentrating on negative thoughts and actions is what leads to a disorder in the first place.
Book a free 30-minute consultation with an Acceptance and Commitment Therapy specialist.